How to Care for Your Dental Implants: Essential Tips for Long-Lasting Results and Maintenance

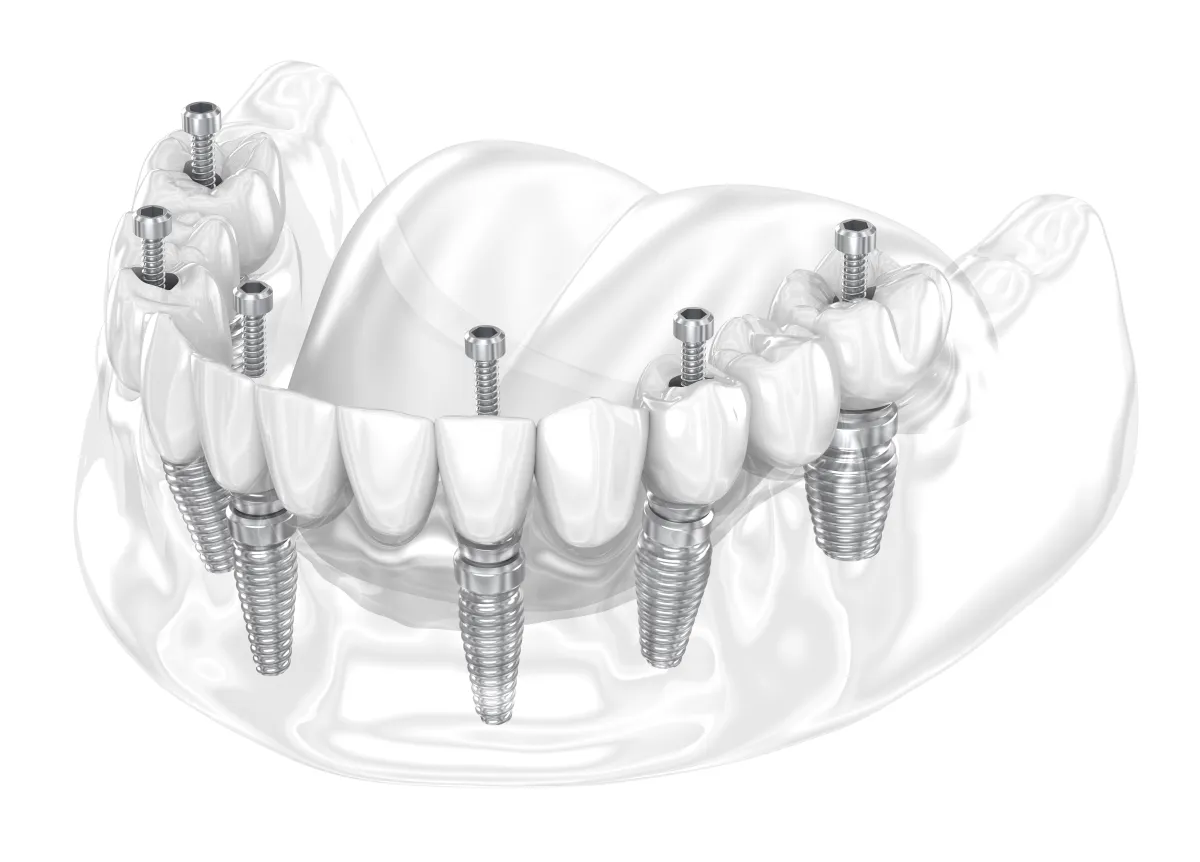
Maintaining dental implants demands a precise balance of daily hygiene, professional oversight, and lifestyle choices to preserve implant stability and oral health. Patients often worry about implant failure, infections, or bone loss; this guide promises clear, expert-backed solutions to protect your investment. You’ll explore why proper care matters, step-by-step cleaning routines, recommended check-up schedules, diet and habits that support longevity, how to spot complications early, and the best tools for at-home maintenance—all informed by Dental Care Rialto’s patient-centered approach.
Why Is Proper Dental Implant Care Crucial for Longevity?
Dental implant care encompasses daily plaque removal, tissue health preservation, and professional monitoring to prevent inflammatory conditions while promoting osseointegration and long-term stability. Effective maintenance reduces bacterial colonization around the implant-abutment interface, which directly enhances implant success rates and supports jawbone integrity.
Dental implant care offers three primary longevity benefits:
1.Enhanced osseointegration supports stronger bone anchorage.
2.Reduced risk of peri-implantitis preserves surrounding gum tissue.
3.Improved function and aesthetics ensure lasting comfort and confidence.
What Are the Benefits of Maintaining Dental Implants?
Regular maintenance improves chewing efficiency, protects adjacent teeth, and supports overall oral health by preventing bone resorption and soft-tissue inflammation. For example, consistent plaque removal promotes healthier gums, which in turn stabilizes the implant and supports adjacent natural teeth.
How Does Oral Hygiene Impact Dental Implant Health?
Effective oral hygiene removes biofilm around the crown and abutment, preventing bacterial penetration into the peri-implant sulcus. Brushing, flossing, and antimicrobial rinses work together to inhibit pathogenic microflora, fostering tissue health and reducing inflammation.
How Does Jawbone Density Influence Implant Eligibility

The Impact of Oral Hygiene on the Success of Dental Implant Prosthetics / Implant Maintenance: A Clinical Update
Effective daily oral hygiene, including brushing twice daily, can significantly reduce the likelihood of peri-implantitis by 70% to 80%. Regular professional maintenance visits, ideally every three to four months, are also crucial for detecting early complications and removing plaque and calculus that at-home care cannot address, thereby preserving peri-implant tissue health and preventing disease progression.
This research reinforces the article's recommendations for diligent daily cleaning routines and the necessity of consistent professional dental check-ups for long-term implant health and the prevention of complications like peri-implantitis.
What Risks Arise from Neglecting Implant Care?
Skipping proper cleaning or professional visits can lead to peri-implantitis, characterized by bleeding, swelling, and progressive bone loss, which ultimately jeopardizes implant stability. Untreated inflammation increases the likelihood of implant loosening and failure.
What Is the Best Daily Cleaning Routine for Dental Implants?
An effective daily routine combines gentle brushing, targeted interdental cleaning, and antimicrobial rinses to disrupt plaque formation, protect soft tissues, and maintain a healthy implant interface. Following these steps prevents infection and preserves implant-to-bone integration.
How Should You Brush Dental Implants Properly?
1.Select a soft-bristled or specially designed implant brush.
2.Angle bristles at 45° toward the gum line, gently moving in short strokes around the crown.
3.Brush all surfaces of the implant crown and adjacent teeth for at least two minutes.
4.Rinse thoroughly and inspect the abutment for plaque or debris.
This routine supports peri-implant tissue health and reduces inflammation, preparing you to address interdental cleaning next.
What Are the Effective Flossing Methods for Implants?

What Are the Effective Flossing Methods for Implants?
Interdental brushes and water flossers remove debris from the implant-tooth interface:
Interdental Brushes – Gently slide between crown and adjacent teeth to dislodge food particles.
Water Flossers – Direct a low-pressure stream around the implant base to flush out bacteria.
Superfloss – Thread under the implant bridge for thorough sub-gingival cleaning.
Consistent interdental cleansing prevents biofilm buildup and complements brushing for complete hygiene.
Which Mouthwashes Are Recommended for Implant Care?
Using antimicrobial, non-alcoholic mouthwash helps reduce bacterial load without irritating tissues. Look for chlorhexidine gluconate or essential-oil formulations that neutralize pathogens around the implant abutment. Rinse twice daily for thirty seconds to reinforce mechanical cleaning steps.
How Often Should You Schedule Professional Dental Implant Maintenance?
Professional care involves specialized instruments and clinical expertise to detect early complications and perform deep cleaning that home routines cannot achieve. These visits preserve implant integrity and intercept issues before they advance.
Why Are Regular Dental Check-ups Important for Implants?
Your dentist evaluates gum health, measures pocket depths around implants, and identifies plaque or calculus in hard-to-reach areas. Early detection of inflammation, loosening, or bone loss enables timely interventions that protect implant longevity.
What Specialized Tools Do Dentists Use for Implant Cleaning?
Dental professionals employ instruments designed to avoid scratching implant surfaces while removing deposits:
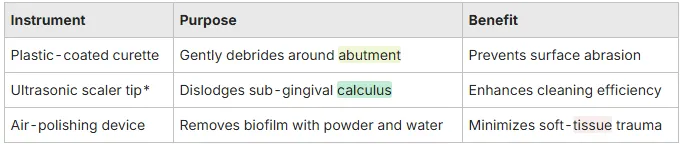
*Scaler tips are specially coated to safeguard implant surfaces. Regular professional cleanings with these tools maintain implant surface integrity and surrounding tissue health.
How Are Early Signs of Implant Complications Identified and Treated?
Inflammatory markers like redness, bleeding on probing, or increased pocket depth signal potential peri-implantitis. Your dentist may perform mechanical debridement, prescribe localized antibiotics, or adjust occlusion to alleviate stress on the implant site.
What Diet and Lifestyle Choices Support Dental Implant Longevity?
Nutrition and habits influence tissue healing, bone density, and microbial ecology around implants. A balanced diet and healthy routines strengthen immune response, reduce inflammation, and support the osseous integration essential for implant success.
Which Foods Should You Avoid to Protect Your Implants?
-Hard items (ice, nuts, hard candy) that exert excessive force on the crown
-Sticky sweets (caramel, taffy) that cling to surfaces and promote plaque
-Staining beverages (coffee, red wine) to reduce discoloration around the implant
Steering clear of these foods prevents mechanical stress and microbial accumulation.
What Are the Best Foods for Oral and Implant Health?
-Leafy greens (spinach, kale) rich in calcium and vitamin K for bone support
-Dairy products (yogurt, cheese) that supply casein and calcium for enamel and bone maintenance
-Lean proteins (fish, poultry) that provide amino acids essential for tissue repair
These foods enhance bone metabolism and gum tissue resilience after implant placement.
How Does Smoking Affect Dental Implant Success?
Smoking introduces toxins that impair blood flow, reduce healing capacity, and elevate infection risk around implants. Nicotine constricts vessels, hindering osseointegration and increasing the likelihood of peri-implantitis.
Smoking and Dental Implants: A Systematic Review and Meta-Analysis
Research indicates that dental implants placed in smokers have a significantly higher risk of failure, with one systematic review and meta-analysis reporting a 140.2% increased risk compared to non-smokers. Smoking also contributes to increased marginal bone loss around implants, affecting both early and late stages of implant integration and survival.
This research directly supports the article's warning about the detrimental effects of smoking on dental implant success and longevity, emphasizing the increased risk of failure and bone loss.
How Can You Recognize and Prevent Common Dental Implant Complications?
Awareness of early warning signs and preventive measures ensures timely management of conditions that threaten implant survival. Routine care and lifestyle modifications play pivotal roles in complication prevention.
What Is Peri-implantitis and How Can You Spot Its Symptoms?
Peri-implantitis is an inflammatory disorder of the tissues surrounding an implant marked by bleeding, swelling, and bone loss. Patients often report tenderness or discharge around the crown, which requires prompt professional intervention to halt progression.
What Are the Signs of Dental Implant Failure?
-Persistent mobility or wobbling of the implant
-Chronic pain or discomfort around the implant site
-Visible bone recession around the implant neck
Identifying these signs early allows for corrective measures before irreversible damage occurs.
How Does Bone Loss Affect Dental Implants and What Can Be Done?
Bone resorption undermines the implant’s structural support and can lead to loosening. Treatments such as bone grafting, guided tissue regeneration, and occlusal adjustments restore bone volume and reestablish implant stability.
What Are the Most Common Questions About Dental Implant Care?
How Do You Clean Dental Implants Daily?
Daily cleaning combines gentle brushing with a soft-bristled or implant-specific toothbrush, interdental cleaning with a water flosser or brush, and an antimicrobial rinse to remove plaque at the crown-abutment junction and maintain tissue health.
What Should You Avoid Doing with Dental Implants?
Avoid abrasive toothpastes, hard-bristled brushes, chewing hard objects, and smoking because these actions can damage implant components, irritate surrounding tissues, and elevate the risk of inflammation.
How Often Should Implants Be Professionally Cleaned?
Most patients benefit from professional implant cleanings every six months; individuals with a history of gum disease or higher risk factors may require visits every three to four months for optimal maintenance.
Can Dental Implants Get Cavities?
No, titanium implants cannot develop cavities, but the surrounding gum tissue and adjacent natural teeth remain susceptible to decay and gum disease, which can indirectly compromise implant health.
What Is the Typical Lifespan of a Dental Implant?
With diligent care, regular professional maintenance, and healthy lifestyle habits, dental implants can last 20 years or more, exhibiting success rates above 95 percent over the long term.
When Should You Contact Your Dentist About Dental Implant Concerns?
What Symptoms Require Immediate Dental Attention?
-Uncontrolled bleeding or severe pain around the implant
-Sudden implant mobility or loosening
-Swelling, fever, or pus discharge indicative of acute infection
Prompt professional evaluation prevents escalation of complications.
How to Prepare for Your Dental Implant Maintenance Appointment?
-Note any changes in implant comfort, mobility, or tissue appearance.
-Bring an updated list of current medications and systemic health changes.
-Avoid eating at least one hour before your visit to facilitate examination.
-Prepare questions about new symptoms or concerns to maximize appointment value.
This preparation enables your dentist to address issues efficiently and reinforce implant longevity.
What Are the Best Tools and Products for Maintaining Dental Implants at Home?
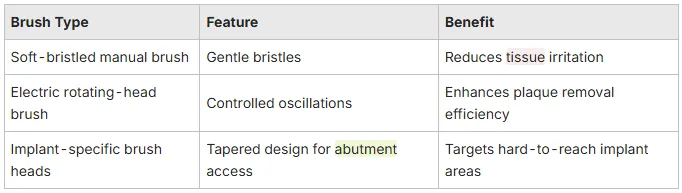
Which Toothbrushes Are Recommended for Dental Implants?
How Effective Are Water Flossers for Implant Cleaning?
Water flossers deliver a targeted stream of water that disrupts bacterial colonies around the implant neck and interproximal spaces, promoting cleaner surfaces without mechanical abrasion. Using a low-pressure setting twice daily supports gingival health and complements brushing.
What Oral Rinses Support Implant Health?
Antimicrobial rinses containing chlorhexidine gluconate or essential oils reduce pathogenic flora around implants without irritating tissues. Rinse for 30 seconds after brushing to maintain a balanced oral microbiome and minimize infection risk.
By following this comprehensive guide—from daily routines to professional check-ups, diet and lifestyle adjustments, complication recognition, and tool selection—you promote the health and durability of your dental implants. For personalized care and expert maintenance, schedule your implant consultation with Dental Care Rialto -Family Dentist in Rialto, CA today.
Are There Patient Testimonials or Success Stories from Rialto Residents?
Many Rialto families share how implants restored their confidence and oral function. One local patient regained full chewing ability after years of discomfort, illustrating the life-changing impact of a well-executed implant restoration. See why residents of Southern California LOVE Dental Care of Rialto here
Sunday - Closed
Monday - 9:30 AM–5 PM
Tuesday -9:30 AM–5 PM
Wednesday - 9 AM–5 PM
Thursday - 9:30 AM–5 PM
Friday - 9 AM–3 PM
Saturday - Closed