Dental Implants in Rialto — Restoring Smiles with Confidence
At Dental Care of Rialto, dental implant surgery replaces missing teeth by placing a biocompatible post into the jawbone. That post bonds with bone through osseointegration and supports a crown or denture so you can chew, speak, and smile more naturally. This guide explains how implant placement works, the common implant options—single-tooth implants, mini implants, and All-on-4 full-arch restorations—and practical details about candidacy, bone grafting, and recovery. Many people who struggle with loose dentures, trouble chewing, or progressive jawbone loss find implants offer a long-lasting, functional solution that preserves facial structure and quality of life. We’ll walk you through the surgical pathway from your first consultation to the final restoration, explain the main cost drivers in Rialto, and help you compare treatment choices so you can decide with confidence. After covering clinical basics, we compare implants with dentures and bridges, outline typical healing timelines, review financing and local care options, and point out how to arrange a free consultation in Rialto.

What Are Dental Implants and How Do They Replace Missing Teeth?
Dental implants act as artificial tooth roots—usually made from titanium or zirconia—placed into the jaw to support an abutment and a crown or denture. Success depends on osseointegration, the natural process where bone bonds to the implant surface. That bond lets chewing forces be transferred into the jaw, which helps maintain bone volume and facial contours. An implant restoration has three parts: the implant post (fixture), the abutment that connects to it, and the crown or denture that restores bite and appearance. Compared with removable prostheses, implants generally improve chewing, stabilize speech, and protect facial shape. Knowing how implants integrate with bone lays the foundation for understanding the steps involved in implant placement and what to expect before, during, and after surgery.
What Is the Dental Implant Procedure and How Does It Work?
Treatment starts with a consultation and diagnostic imaging—often X‑rays or a CBCT scan—to evaluate bone volume and plan precise implant positioning. During the procedure the implant is placed into prepared bone under local anesthesia (or with sedation when needed), and a healing cap or cover screw protects the site while early healing occurs. Over the following weeks to months osseointegration takes place; once the implant is stable the abutment and final crown, bridge, or denture are attached. Whether we load the restoration immediately or wait depends on bone quality, implant stability, and the planned prosthesis. Modern techniques aim to reduce surgical trauma and improve predictability. We know patients often worry about pain and timing—clear communication and a tailored treatment plan help ease uncertainty and support smooth recovery.
How Do Dental Implants Integrate with the Jawbone?
Osseointegration is the process by which bone grows onto the implant surface, generally taking about 3–6 months depending on bone quality and overall health. Once integrated, the implant becomes a stable foundation for the final prosthesis. Normal chewing stimulates bone remodeling around the implant, which helps preserve the height of the ridge and prevents the resorption that follows tooth loss. Factors that can impair integration include active gum disease, heavy smoking, uncontrolled metabolic conditions, or insufficient bone volume. When bone is lacking, we may recommend bone grafting or a sinus lift to rebuild volume—these procedures lengthen the timeline but improve long-term success. Understanding how integration works helps you and your clinician choose materials, surface treatments, and staging that give the best chance for a predictable outcome.
Next, we compare the common implant types and when each is appropriate.
What Types of Dental Implants Are Available for Tooth Replacement?
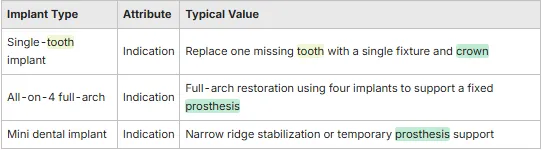
Implant options address a range of needs—from replacing a single tooth to restoring an entire arch. Endosteal single‑tooth implants are the standard for replacing one missing tooth. Mini dental implants can help where the ridge is narrow or for temporary denture stabilization. All‑on‑4 uses four strategically placed implants to support a fixed full‑arch prosthesis for patients with extensive tooth loss. Implant-supported dentures and implant-retained bridges fall between those solutions, offering added stability for patients who find traditional dentures unsatisfactory. The right choice depends on bone volume, bite forces, aesthetic goals, and personal preferences; a candidacy assessment with CBCT imaging guides the recommendation. The table below gives a clear comparison of typical options.
This overview shows how each implant type meets different clinical needs and sets up a detailed candidacy discussion.
In short, implant dentistry scales from single‑tooth fixes to full‑arch reconstructions; the next section explains All‑on‑4 in practical terms.
Common implant categories include single‑tooth implants, All‑on‑4 full‑arch restorations, and mini implants for specific anatomical needs.
Each option balances surgical complexity, recovery time, and prosthetic durability based on the patient’s goals.
3D imaging and a diagnostic plan help determine which implant type will deliver predictable function and aesthetics.
These options illustrate how implant care can be customized from one tooth to an entire smile.
What Are All-on-4 Dental Implants and Who Are They For?
All‑on‑4 is a full‑arch solution that supports a fixed prosthesis on four strategically angled implants, often allowing an immediate provisional prosthesis so patients regain function faster. Ideal candidates are those with many failing or missing teeth who want a stable, fixed restoration without placing a large number of implants, and who have adequate bone in the anterior regions or can accept limited grafting. Benefits include shorter treatment time and fewer surgical sites compared with some full‑arch approaches, while trade‑offs include prosthetic maintenance over time and load management. Immediate loading depends on primary stability and prosthetic planning. We discuss follow‑up care and maintenance so patients understand long‑term expectations and how All‑on‑4 compares with other full‑arch strategies.
How Do Mini and Single Tooth Implants Differ?
Mini dental implants are narrower and useful for narrow ridges, denture stabilization, or when a less invasive, lower‑cost option is preferred. Standard single‑tooth implants use wider fixtures that tolerate higher bite forces and typically offer greater long‑term durability. Mini implants often mean quicker short‑term recovery but may not perform as well under heavy occlusal loads over many years. Single‑tooth implants usually pair with ceramic crowns for the best esthetic results when bone is sufficient. Choosing between mini and standard implants depends on functional demands, bone anatomy, and your long‑term restorative goals.
Here are the main differences to consider:
Diameter and strength: Mini implants are narrower and less load‑tolerant than standard single‑tooth implants.
surgical complexity: Mini implants often require less invasive placement than standard implants.
Longevity considerations: Standard implants typically provide superior durability in high‑load areas like molars.
These points help set realistic expectations for performance, cost, and future maintenance.
What Are the Benefits of Dental Implants Compared to Dentures and Bridges?
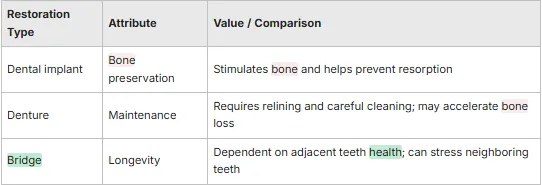
Dental implants help preserve jawbone because they transmit chewing forces into the alveolar bone, slowing the resorption that follows tooth loss. That preservation supports facial contours in a way conventional dentures, which rest on the ridge, cannot. Functionally, implants restore chewing efficiency and speech stability closer to natural teeth, reducing dietary limits and eliminating many of the issues caused by slipping prostheses. Implants also tend to offer longer service life and straightforward hygiene routines; crowns and implant‑supported prostheses can last many years with good care, whereas bridges and dentures may need more frequent replacement or relining. The table below summarizes key differences to guide your decision.
This comparison explains why many clinicians recommend implants to protect both function and facial structure—even though implants involve surgery and different cost considerations.
Patients frequently report better chewing, a more natural appearance, and greater confidence after implant treatment. Clear expectations and ongoing maintenance are key to achieving those results.
How Do Dental Implants Prevent Jawbone Loss and Preserve Facial Structure?
Implants transfer functional load to the alveolar bone, providing mechanical stimulation that maintains bone remodeling and volume. That stimulation helps preserve the socket and prevents the ridge collapse that commonly follows extraction or long‑term denture use. When bone resorption is minimized, the overlying soft tissues and facial contours remain fuller, reducing the “sunken” look associated with long‑term tooth loss. Clinically, bone preservation makes future restorative options more predictable and improves long‑term aesthetic outcomes. When bone loss has already occurred, grafting and augmentation can rebuild volume and enable implant placement that restores both function and form.
What Functional and Aesthetic Improvements Do Implants Provide?
Implants restore chewing efficiency so most patients can enjoy a wider range of foods again, which supports nutrition and general well‑being. Fixed restorations also reduce speech instability caused by removable prostheses. Aesthetically, implant crowns are matched for color and contour to surrounding teeth, producing a natural smile and boosting self‑confidence. Patient satisfaction is typically high when expectations and maintenance requirements are discussed clearly up front, which is why tailored planning and follow‑up care are part of our process.
How Much Do Dental Implants Cost in Rialto and What Financing Options Are Available?
Implant costs vary with the number of implants, whether bone grafting or a sinus lift is needed, the implant system and materials selected, and laboratory fees for crowns or prostheses. Single‑tooth implant with a crown generally falls in a mid‑to‑high range compared with simpler restorations because it includes surgery, components, and lab work. Full‑arch options like All‑on‑4 change the cost structure by spreading prosthetic costs across fewer fixtures. Common financing choices include staged payments, third‑party healthcare financing, or phasing treatment to spread expense. We provide transparent pricing discussions and a free consultation so families in Rialto and nearby cities can review individualized treatment plans and financing before deciding on surgery.
This breakdown helps explain why estimates differ and underscores the value of a personalized quote during your consultation.
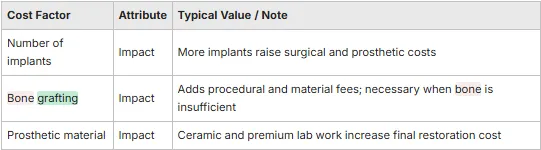
What Factors Influence the Cost of Dental Implant Surgery?
Major cost drivers include surgical complexity (single implants versus full‑arch reconstructions), any ancillary procedures like extractions or grafts, the implant system and materials chosen, and lab fees for custom prosthetics. Location and provider expertise also affect price: practices offering advanced imaging, guided surgery, and premium restorative materials may charge more to reflect those services. Insurance coverage varies—many plans limit benefits for implants or treat them differently from bridges—so out‑of‑pocket costs depend on individual policies. Knowing these variables helps you compare offers based on clinical value rather than sticker price alone.
Does Dental Insurance Cover Dental Implants?
Many dental insurance plans limit or exclude full coverage for implants, sometimes covering only parts of related procedures or offering benefits similar to bridge coverage. Some medical plans may help in reconstructive or trauma cases, but coverage is plan‑specific and must be verified. At Dental Care of Rialto we help patients check benefits and discuss alternate financing if insurance support is limited. We recommend a pre‑treatment benefit check and a free consultation so you’ll have a reliable cost estimate and a clear picture of payment options before scheduling treatment.

What Is the Dental Implant Surgery Process and What Should Patients Expect During Recovery?
The implant journey includes evaluation and digital planning, surgical placement of the implant, a healing phase for osseointegration, and the final prosthetic restoration—plus follow‑up visits to monitor healing and hygiene. Preoperative assessment identifies medical or oral factors—like gum disease or low bone volume—that should be managed first to improve success. Pain control strategies, antibiotics or antiseptic rinses when indicated, and clear post‑op instructions help reduce complications and keep you comfortable during early healing. The numbered steps below summarize the clinical flow so you know what to
expect before we cover recovery specifics.
Consultation and imaging: Diagnostic scans and treatment planning determine candidacy and implant placement strategy.
Surgical placement: Implant fixtures are placed into bone under local anesthesia or sedation, with soft tissue managed for optimal healing.
Healing and restoration: After osseointegration, abutments and final crowns or bridges are attached to restore chewing and aesthetics.
This stepwise view prepares you for the sequence of events and decision points at each stage of treatment.
What Are the Key Steps in Dental Implant Surgery?
The process begins with a full consultation that includes your medical history and 3D imaging to evaluate bone anatomy and map implant positions. Surgery follows—our team prepares the site, places the implant, and closes or covers the area to promote healing; immediate provisional restorations are possible in selected cases. You’ll then enter the osseointegration phase, during which routine follow‑ups check stability and soft‑tissue healing. Once integration is confirmed, we fabricate and attach the abutment and final prosthesis to complete the restoration. Each stage may include decisions—such as grafting or immediate loading—that affect timing and outcomes.
How Long Is the Recovery Timeline and What Is Post-Operative Care?
Immediately after surgery most patients experience mild swelling and tenderness for 24–72 hours, manageable with pain medication, cold packs, and rest. Sutures typically dissolve or are removed within one to two weeks. Soft tissues usually stabilize in 1–2 weeks, but full osseointegration—the secure bonding of implant and bone—typically takes 3–6 months, depending on bone quality and overall health. Long‑term care includes gentle oral hygiene, avoiding hard foods on the implant during early healing, and regular dental visits for maintenance and prosthetic checks. Watch for warning signs such as persistent swelling, uncontrolled pain, fever, or prosthetic instability, and contact your clinician promptly if they occur.
Quick postoperative checklist:
Stick to a soft diet and avoid chewing on the surgical site for the first few days.
Keep oral hygiene gentle around the area and use any recommended antiseptic rinses.
Attend follow‑up visits for suture checks, healing assessments, and prosthetic planning.
Following these steps helps reduce complications and supports predictable integration and restoration.
Why Choose Dental Care of Rialto and Dr. Carmy for Your Dental Implant Needs?
Dental Care of Rialto delivers family‑focused implant services to Rialto and nearby communities—San Bernardino, Rancho Cucamonga, Riverside, and Fontana—combining modern techniques with individualized treatment planning to restore function and smiles. Dr. Carmy brings recognized implant expertise and teaches at the Dental Implant Institute (DII), which keeps our practice current with contemporary surgical protocols and evidence‑informed care. We emphasize compassionate, family‑centered planning, offer state‑of‑the‑art implant options—including single implants, mini implants, and All‑on‑4—and start care with a free consultation to review personalized plans and financing. Local families benefit from our focus on detailed diagnostics and consistent follow‑up that supports long‑term implant health.
What Makes Dr. Carmy a Leading Expert in Dental Implantology?
Dr. Carmy’s role training other dentists at the Dental Implant Institute highlights a commitment to teaching current implant techniques and delivering predictable surgical results in practice. That instructional work keeps him engaged with evolving protocols, implant systems, and digital planning workflows—all of which inform patient care decisions. Dr. Carmy emphasizes evidence‑based planning and individualized sequencing to minimize surprises and improve prosthetic outcomes. If you’d like to learn more about credentials and clinical philosophy, request a consultation to see how that expertise applies to your treatment plan.
How Does Dental Care of Rialto Provide Personalized and Advanced Implant Care?
We build treatment plans around each patient’s anatomy, function, and family needs, using modern imaging, restorative materials, and procedural options to tailor care. Practical supports include a free initial consultation to review candidacy, transparent conversations about timelines and costs, and flexible staging to match your schedule and budget. Our family‑centered approach coordinates care across ages and emphasizes clear post‑op guidance and maintenance plans to protect long‑term results. For Rialto residents, combining advanced techniques with local access helps turn implant science into dependable everyday function.
Local service: We serve Rialto and nearby cities to make implant care accessible.
Personalized planning: Treatment plans address bone anatomy, prosthetic goals, and family needs.
Free consultation: A no‑cost consult clarifies candidacy, cost estimates, and financing before treatment.
This section positions Dental Care of Rialto as a local, evidence‑informed practice that keeps patient education central to decision‑making.
Frequently Asked Questions
1. What is the typical recovery time after dental implant surgery?
Recovery varies by patient. Typically the initial healing phase lasts 1–2 weeks for soft tissues, with mild swelling and discomfort that resolve in a few days. Full osseointegration—the implant bonding with bone—usually takes 3–6 months. During this period follow post‑op instructions, maintain a soft diet when advised, and attend follow‑up visits. Individual factors such as bone quality and overall health can affect timing.
2. Are there any risks or complications associated with dental implants?
As with any surgery, implants carry risks. Possible complications include infection at the site, nerve irritation, or sinus issues when placing implants in the upper jaw. Failure to integrate can occur if bone density is inadequate or systemic conditions interfere with healing. Discuss your medical history and concerns with us so we can minimize risks and plan for the best outcome.
3. How long do dental implants typically last?
Implants are designed as a long‑term solution and can last 10–15 years or longer with proper care. Longevity depends on oral hygiene, regular dental checkups, and lifestyle factors like smoking. While the titanium or zirconia implant may last decades, the prosthetic crown or denture may wear and require replacement. Consistent maintenance maximizes lifespan.
4. Can anyone get dental implants, or are there specific requirements?
Many people are candidates, but certain requirements apply. Ideal candidates have sufficient bone to support an implant and healthy gums without active periodontal disease. Chronic conditions (for example, uncontrolled diabetes) and smoking can affect success. A thorough evaluation with imaging will determine candidacy and whether preparatory procedures, such as bone grafting, are needed.
5. What should I expect during the dental implant consultation?
At the consultation we review your medical history, examine your mouth, and take diagnostic images (X‑rays or 3D scans) to assess bone and plan implant placement. We’ll discuss treatment options, expected timelines, costs, and any preparatory steps. This is a good time to ask questions and share concerns so we can craft a plan that fits your needs.
6. How do I care for my dental implants after surgery?
Post‑op care is essential. Maintain a soft diet for the first few days, avoid hard or chewy foods near the surgical site, and follow gentle oral hygiene instructions. Use any prescribed antiseptic rinses and keep follow‑up appointments to monitor healing. Be alert for signs of complications—persistent pain, swelling, or fever—and contact us if anything concerns you.
Sunday - Closed
Monday - 9:30 AM–5 PM
Tuesday -9:30 AM–5 PM
Wednesday - 9 AM–5 PM
Thursday - 9:30 AM–5 PM
Friday - 9 AM–3 PM
Saturday - Closed